Brussels 19 December 2015. National and European research funding in the field of antibacterial resistance is unbalanced and underfunded, according to new research by the Joint Programming Initiative on Antimicrobial Resistance (JPIAMR) published in the journal Lancet Infectious Diseases today. The study, which is the first of its kind, highlights the need for increased and new investment across all Member States. The work was led by the UK‘s Medical Research Council (MRC).
The study mapped out antibacterial resistance research undertaken across 19 countries from 2007-2013, identifying 1,243 projects with a total public investment of €1.3 billion. The study looked at national investments and European Union organisations investments, including the European Commission’s investment in the Innovative Medicines Initiative (IMI) and found that funding varies considerably across countries and within the different research areas. The 19 countries covered by the study are Belgium, Canada, Czech Republic, Denmark, Estonia, Finland, Germany, Israel, Italy, The Netherlands, Norway, Poland, Romania, Spain, Sweden, Switzerland, Turkey and the UK.
Antibiotic resistance has been highlighted as one of the main threats to human health worldwide. In 2007 alone, 25,000 patients died in Europe from infections caused by bacteria that were resistant to more than one antibiotic – and current trends predict this to grow to 390,000 deaths a year by 2050.
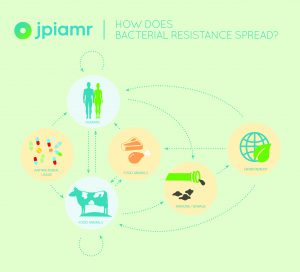
In order to address antimicrobial resistance, research across a wide range of areas in humans, animals, and the environment is critical. There is a need to develop new and preserve existing antibiotics and alternatives to antibiotics, improve diagnosis to reduce unnecessary and inappropriate antibiotic prescribing, implement surveillance systems to monitor resistance and antibiotic use, understand the development and transmission of resistance, and improve infection prevention and control strategies. The Lancet study is the first systematic study to look at national and European Union funding in antibacterial resistance across a range of research areas in order to identify gaps and opportunities to be exploited.
The JPIAMR mapping study has shown that across 19 countries from 2007-2013, 66% of funding was awarded to projects in the field of therapeutics. This is a stark contrast to the other fields such as transmission, which received 9% of the funding, 14% of funding went to diagnostics, 5% to interventions and only 2% awarded to projects on antimicrobial resistance in the environment and 4% in surveillance.
“Funds have been invested in AMR research, however this study clearly shows us a gap between the funding of studies needed to reduce resistance and the actual research funded. As well as increased funding, we need to tackle this growing concern together, by strengthening national and international collaborations, co-ordinating research activities, and combining resources “ said Mats Ulfendahl, Chair of JPIAMR’s Management Board.
91% (1,129/1,243) of projects identified in this study were funded at national level. However, they only accounted for 49% of total investment, suggesting that these are relatively small awards and highly focussed projects.
“National research investment is too low compared to that committed at European Union level. To achieve greater impact, nations need to come together and pool available resources. This entails working together in a more efficient way to increase the impact of research through strengthening national and international coordination and collaborations as well as harmonising research activities and national strategies. The results demonstrate the need for a Joint Programming Initiative on Antimicrobial Resistance,” said Herman Goossens, Chair of JPIAMR’s Science Advisor Board.
Notes to editors:
Media contacts:
Sofia Kuhn, JPIAMR communications
Email: sofia.kuhn@vr.se
Phone: +32 486 67 39 42
Link to paper (open source): http://dx.doi.org/10.1016/ S1473-3099(15)00350-3
Ruth Kelly, MPH, Ghada Zoubiane, PhD, Desmond Walsh, PhD, Rebecca Ward, PhD, Prof Herman Goossens. Lancet Infectious Diseases (Dec 2015). Public funding for research on antibacterial resistance in the JPIAMR countries, the European Commission, and related European Union agencies: a systematic observational analysis
Further information
Currently, there is no comprehensive database to document research at both national and international levels, and from conducting this work it is clear that improvements in data sharing and communication need to be achieved at national level in several countries. The JPIAMR is actively working to improve this and has turned the research data collected for this work into a useful, freely accessible, and searchable database available on the JPIAMR website. This will enable researchers and funders to determine what has already been funded across the different areas and determine what is yet required in order to set strategic priorities. It is likewise hoped that it will be used by researchers for networking and collaboration and to avoid duplication. If funders from other countries provide similarly detailed information of projects on ABR research, global gaps and priorities could be assessed.
About JPIAMR
The Joint Programming Initiative on Antimicrobial Resistance (JPIAMR) joins forces across nations to fight AMR through effective collaborative actions in areas of unmet needs. A shared common research agenda enhances multi-disciplinary collaboration and ensures that knowledge gaps are quickly identified and filled.
At the moment, European AMR funding is skew towards research in therapeutics, largely ignoring other areas such as transmission dynamics and the impact of the environment, crucial areas to understand in order to reduce resistance.
The gap between research funding into chronic diseases and antimicrobial resistance is large but difficult to document. However, national AMR funding does exist but is relatively small and targeted. In addition, countries with low national AMR prevalence allocate more money towards research than countries with greater needs for AMR solutions. This suggests a need for greater coordination across Europe in order to fill knowledge gaps.
JPIAMR coordinates national funding and supports collaborative action to fill existing knowledge gaps. The goal is to shape cohesive and coordinated AMR funding and actions that maximise on resources and reduce duplication of research. Mobilising existing and new resources will create a greater critical mass and attract new researchers into the AMR field. A Strategic Research Agenda (SRA), which outlines key [neglected] areas to tackle, guides JPIAMR and focuses research actions.
JPIAMR cannot address all aspects of the AMR problem, but can show a way forward by producing new research, engaging new researchers and creating networks that create long-term momentum for other areas in society. There is an urgent need for interdisciplinary and public-private partnerships to support research in the antimicrobial resistance area. Exchanges between industry, public health bodies, and academic bodies will entail not only sharing costs, but also coordination of the respective research activities. This is where JPIAMR will make a difference.
To date 22 countries have joined forces in the Joint Programming Initiative on Antimicrobial Resistance.
utveckling.jpiamr.eu
About MRC
The Medical Research Council is at the forefront of scientific discovery to improve human health. Founded in 1913 to tackle tuberculosis, the MRC now invests taxpayers’ money in some of the best medical research in the world across every area of health. Thirty-one MRC-funded researchers have won Nobel prizes in a wide range of disciplines, and MRC scientists have been behind such diverse discoveries as vitamins, the structure of DNA and the link between smoking and cancer, as well as achievements such as pioneering the use of randomised controlled trials, the invention of MRI scanning, and the development of a group of antibodies used in the making of some of the most successful drugs ever developed. Today, MRC-funded scientists tackle some of the greatest health problems facing humanity in the 21st century, from the rising tide of chronic diseases associated with ageing to the threats posed by rapidly mutating micro-organisms.
www.mrc.ac.uk